
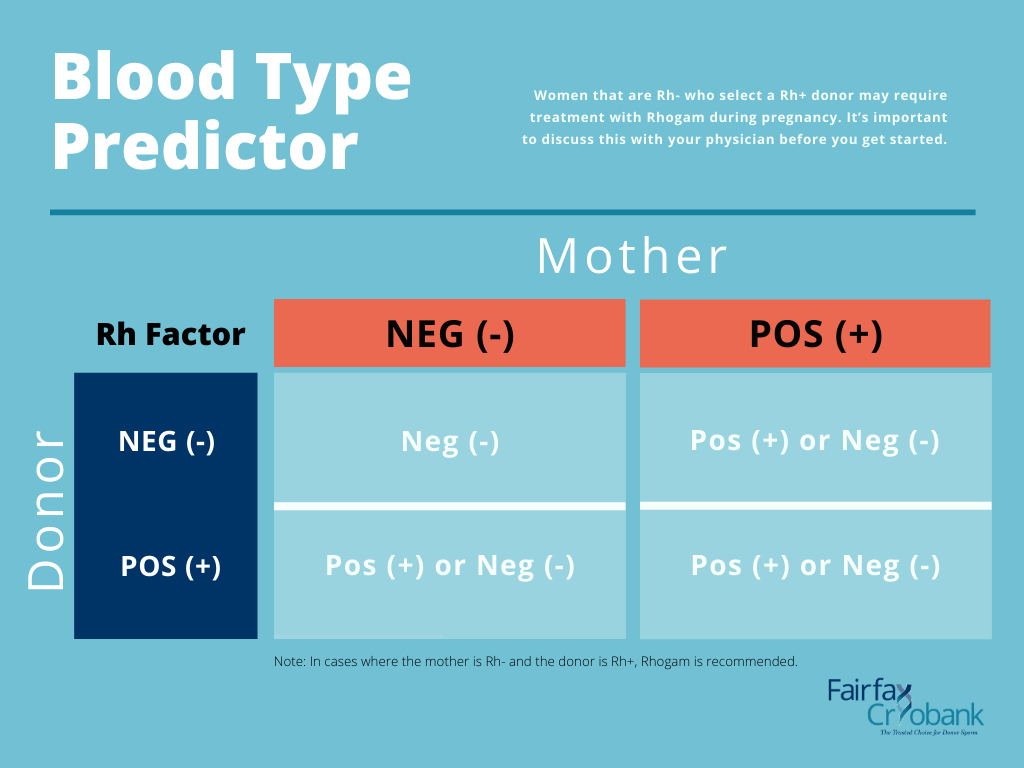
How do you know if you are Rh negative?Ī simple blood test can show if you are Rh negative. This can cause health risks for that fetus and for the fetus of any subsequent pregnancies she may have.Ī pregnant woman who is Rh negative, who has a fetus which is Rh negative won’t have any problems.Ī pregnant woman who is Rh positive won’t have any problems (with antibodies to RhD), regardless of whether the baby is Rh positive or negative. These antibodies then attack the unborn baby’s red blood cells. But when a mother is Rh negative and her fetus is Rh positive, the mother’s blood may produce antibodies against the baby’s Rh factor. On its own the Rh factor does not cause health problems. Mild transfusion reactions are not dangerous, but a severe transfusion reaction may be deadly. But if an Rh negative (RhD-) person receives Rh positive (RhD+) blood, their body reacts, making chemicals (antibodies) to defend against the foreign Rh factor. If this is not available, they may be given blood from a compatible blood group. Otherwise a reaction to the ‘foreign’ blood may occur. When someone needs a blood transfusion it is preferable that they are transfused with blood from the same ABO and RhD groups as their own. For example, someone’s blood may be ‘O positive’ (written O+) and another person may be ‘AB negative’ (written AB-).
A NEGATIVE BLOOD TYPE DURING PREGNANCY PLUS
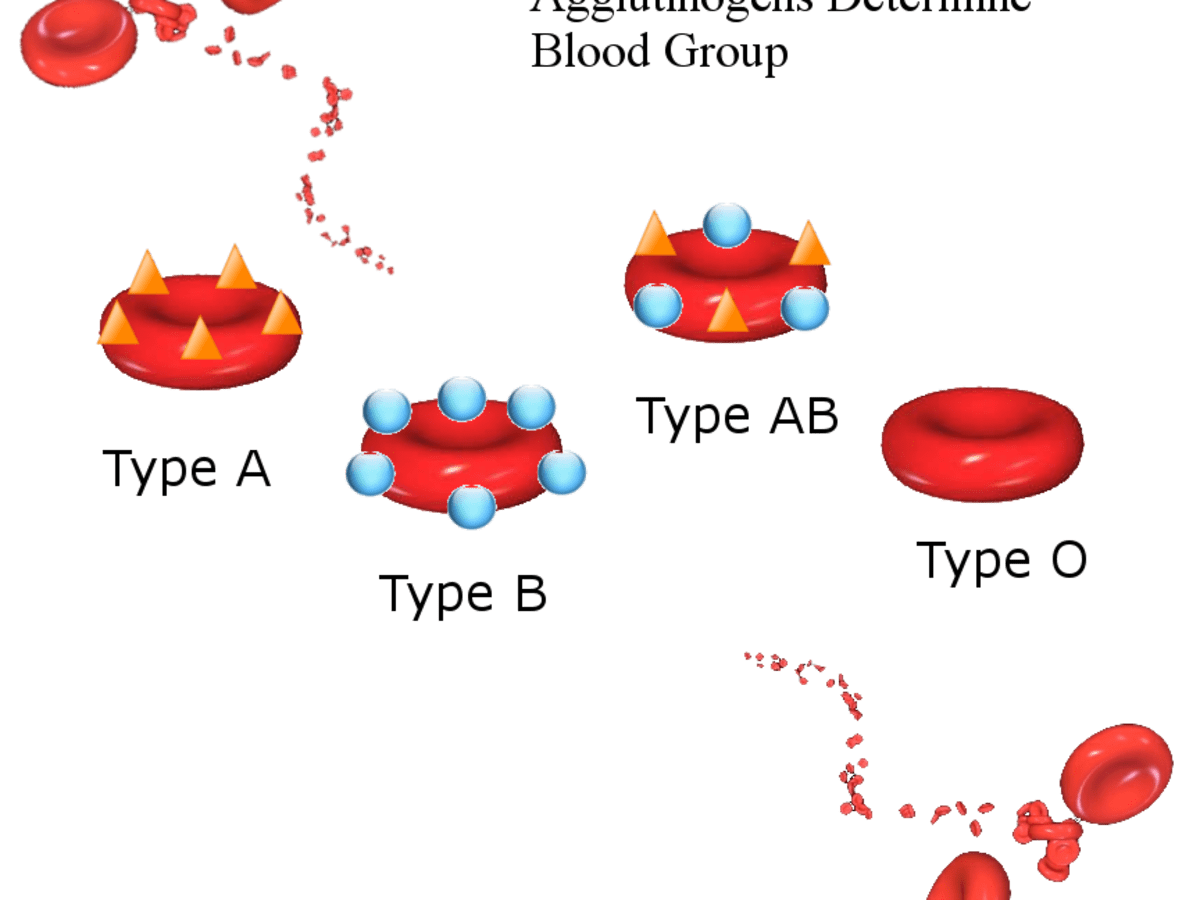
Each blood type is also further identified by a plus (+) or minus (-) sign, which designates the Rh status of the blood. In Australia, around 80 per cent of people are Rh positive.īlood is classified into groups, the most well-known being the ABO system in which a person’s blood is recorded as either A, B, AB or O. Most people have the Rh factor and test Rh positive (RhD+), however, some people don’t have the Rh factor and so are Rh negative (RhD-).

A person’s blood is either Rh positive (has the RhD protein) or Rh negative (doesn’t have the RhD protein). Rhesus factor was originally named (incorrectly) after rhesus monkeys, but now scientists more correctly refer to it as Rh factor. Rhesus factor is an inherited protein called RhD which is found on the surface of red blood cells.

It happens when a rhesus negative woman carries a fetus with rhesus positive (RhD+) blood.įortunately, even though your baby’s blood type is not usually known until delivery, a simple treatment during pregnancy can help prevent problems in women who are RhD negative. Rhesus disease is an incompatibility between the blood types of the mother and the baby. I hope this information is helpful.If you have rhesus negative (RhD-) blood and are pregnant, your fetus may be at risk of health problems caused by rhesus disease. So far my pregnancy is going well🙏🏾but im not letting up on the Oneg rhogam shot asking about it and making sure I received the necessary injections at 28weeks and after baby is born🌈. I think my immune system attacked my 1st pregnancy because it was a new and unrecognized organism and my body did not know what to do with it… those are my thoughts although some drs like to say it is not related but I think to myself how could it not be? The very purpose of the rhogam shot is to tell your existing antibodies not to attack the pregnancy and make new antibodies to keep the pregnancy thriving… with this pregnancy i ask about the rhogam shot at every visit especially since I was spotting early on and was concerned about the baby blood mixing with mine. To this day, I firmly believe that me having an ONeg blood type contributed to my loss. When they ran the analysis on the fetal remains, the doctor wrote in my operational report that they did not find anything genetically abnormal and thus the reason for my MC was inconclusive. i had 2 D&Cs to resolve the MMC (long story) and I had a rhogam shot which is what I think you are referring to as Anti-D after I miscarried and after the D&C. Baby stop growing at 6 weeks and confirmed as a MMC at 8 weeks. Hi there im Oneg 14 weeks tomorrow (3/8) FTM however my first pregnancy in 2019 was a MC.


 0 kommentar(er)
0 kommentar(er)
